
Resident Corner
Anatomical description during standard upper endoscopy
In this video (Figure 1), we demonstrate standard upper endoscopy performed on a 50-year-old patient with history of gastroesophageal (GE) reflux disease and dyspepsia. We highlight the common anatomical landmarks of the upper gastrointestinal tract (Table 1, Figure 2) and endoscopic techniques for successful esophageal intubation, gastric retroflexion, duodenal access and tissue sampling using biopsy forceps.
Figure 1 Anatomical description during standard upper endoscopy (1). Available online: http://aos.amegroups.com/post/view/1550051583

Table 1 Anatomical location and commonly encountered pathology
Full table
Full table
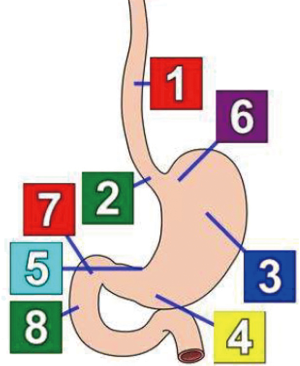
Figure 2 Anatomical landmarks during upper endoscopy. Label 1: mid-esophagus; label 2: gastroesophageal junction; label 3: gastric body; label 4: gastric antrum; label 5: incisura; label 6: gastric fundus; label 7: duodenal bulb; label 8: second part of duodenum.
Essentials of endoscopic reporting
Esophagus
- Z line: regular vs. irregular;
- Location of GE junction from incisors (example: 40 cm);
- Ease of scope passage through GE junction;
- If varices present: grade, size, location, red wale sign or white nipple sign (stigmata of bleeding);
- Hiatal Hernia: size, from GE junction to diaphragmatic pinch (example 35–40 cm), Hill classification;
- Esophagitis: Los Angele (LA) Grading/Classification;
- Barrett’s esophagus: length, Prague classification.
Stomach
- Presence of ulcers, erosions, Cameron lesions, gastric antral vascular ectasia (GAVE) and other mucosal pathology;
- Ulcer: shape, size, clean based, overlying clot, visible vessel, surrounding mucosa appearance;
- Mass: regular vs. irregular, size (measure proximal extension to distal extension), malignant appearing, anterior vs. posterior wall or lesser curvature vs. greater curvature, extension into esophagus or GE junction, spontaneous bleeding or contact bleeding;
- If gastritis is present: location, patchy vs. diffuse, mild vs. severe, contact bleeding vs. spontaneous bleeding.
Duodenum
- Presence of ulcers, duodenitis, villous atrophy, diverticula, and ampullary lesions;
- Ulcer: shape, size, clean based, overlying clot, visible vessel, surrounding mucosa appearance;
- Extent of duodenum evaluation (usually 2nd or 3rd part of duodenum).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Bazarbashi AN, Hathorn KE, Ryou MR. Anatomical description during standard upper endoscopy. Art Surg 2019;3:v002. Available online: http://aos.amegroups.com/post/view/1550051583
doi: 10.21037/aos.2019.03.01
Cite this article as: Bazarbashi AN, Hathorn KE, Ryou M. Anatomical description during standard upper endoscopy. Art Surg 2019;3:2.
Cite this article as: Bazarbashi AN, Hathorn KE, Ryou M. Anatomical description during standard upper endoscopy. Art Surg 2019;3:2.


