
The winner for D2 lymph node dissection in distal gastrectomy—anatomic landmarks vs. number of examined lymph nodes
Introduction
Although D2 lymph node dissection in treating gastric cancer has been considered as a standard care in Asia, the standardization and adoption of this procedure in non-tertiary medical center remains a real challenge. One of the major obstacles is the complexity of the peri-gastric lymph node distribution, perigastric spaces and the relationships among stomach, major blood vessels, colon, pancreas and spleen. For low incidence geographic area, such as in US or Europe, this surgery is even more challenging since most of the centers treat less than 20 cases/year. This manuscript illustrated the anatomical landmarks for D2 lymph node dissection in distal gastrectomy in order to facilitate the learning process and achieve the standardization of this surgical procedure.
Surgical techniques
Indication for distal gastrectomy
Gastric cancer presents at distal of the stomach, most commonly in the pylorus or antrum.
Review the relevant anatomy
For medical student, resident and fellows, please refer to the mini-lecture on this topic at Resident Corner “Gastric lymph node stations” to understand the nomenclature of gastric lymph node stations.
The scope of lymph node dissection
According to Japanese Gastric Cancer Association Gastric Cancer [2017] (1), D2 lymph node dissection included stations: No. 1, 3, 4sb, 4d, 5, 6, 7, 8a, 9, 11p, and 12a (Figure 1).
Anatomic landmark for D2 lymph node dissection (distal gastrectomy)
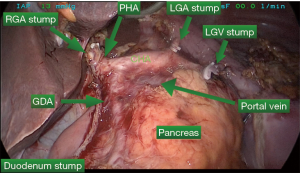
In order to achieve D2 lymph node dissection, the following anatomic landmarks need to be demonstrated (Figure 2):
- The origin of left gastroepiploic artery;
- The origin of right gastroepiploic artery and vein;
- Gastroduodenal artery;
- The origin of right gastric artery;
- The origin of left gastric artery and vein;
- The lateral wall of proper hepatic artery;
- The common hepatic artery, celiac trunk and proximal splenic artery;
- Serosa of the less curvature, the mid-distal portion of the greater curvature.
Surgical approaches
There are many approaches to perform the lymph nodes dissection. Author introduced a six steps D2 lymph node dissection in the following order:
- Greater curvature dissection:
- Take down the gastrocolic ligament;
- Dissection the left gastroepiploic artery;
- Dissection the right gastroepiploic artery.
- Supra-pancreatic dissection;
- Antrum dissection;
- Porta hepatis dissection;
- Posterior stomach dissection;
- Less curvature dissection.
The attached video (Figure 3) “Anatomical landmarks for D2 lymph node dissection in distal gastrectomy” illustrated each step in detail with narratives to explain the tricks and pitfalls.
Discussion
Many of residents and fellows are confused with the concepts of D2 lymph node dissection, excised lymph nodes, and examined lymph nodes. D2 lymph node dissection defines the scope of surgery. The term “excised lymph nodes” refers to the lymph nodes contained in the resected specimen whereas the term “examined lymph nodes” refers to the lymph nodes identified and accessed by pathologists. Although 15 examined lymph nodes are needed to indicate the adequacy of gastric cancer surgery, it has been well recognized that the number of lymph nodes is not a perfect surrogate for the scope and quality of surgery. Number of lymph nodes is related to tumor pathology characteristics, patient’s age, sex, immunologic status, quality of surgery, and pathology examination (3). Therefore, it is important for surgeons to improve the surgical skill and rely on anatomic landmarks instead of number of lymph nodes to evaluate the quality of surgery. This manuscript presents detail techniques, tips, tricks and pitfalls for distal gastrectomy with D2 lymph node dissection. It will help new learners to shorten learning curve and to reduce postoperative c omplications including, pancreatic leak, splenic injury, bowel injury and bleeding.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
References
- Japanese Gastric Cancer Association Gastric Cancer [2017]: Available online” https://doi.org/ [Crossref]
- Wang J. Anatomical landmarks for D2 lymph node dissection in distal gastrectomy. Art Surg 2017;1:v004. Available online: http://aos.amegroups.com/post/view/2017121101
- Wang J, Kulaylat M, Rockette H, et al. Should total number of lymph nodes be used as a quality of care measure for stage III colon cancer? Ann Surg 2009;249:559-63. [Crossref] [PubMed]
Cite this article as: Wang J. The winner for D2 lymph node dissection in distal gastrectomy—anatomic landmarks vs. number of examined lymph nodes. Art Surg 2017;1:8.



